Bradycardia is a heart related problem defined by an abnormally slow heart rate, usually less than 60 beats per minute in adults. While a slower heart rate is acceptable for some people, bradycardia can occasionally indicate an underlying health problem that necessitates medical treatment. In this post, we will look at the causes, symptoms, diagnosis, and treatment options for bradycardia.
Causes of Bradycardia:
There are various possible reasons of bradycardia, including physiological factors, medical problems, and medication. Common causes include:
- Age-related changes: As people age, their hearts’ electrical systems may become less efficient, resulting in a slower heart rate.
- Athletic : High-level athletes may develop bradycardia due to their improved cardiovascular fitness. This is commonly referred to as the “athlete’s heart” and is usually not cause for alarm.
- Heart Disease: Coronary artery disease, myocarditis, heart attacks, and congenital heart anomalies can all interrupt the electrical impulses in the heart, leading in bradycardia.
- Hypothyroidism: An under active thyroid gland can cause a slower heart rate.
- Electrolyte Imbalance: Abnormal amounts of potassium, calcium, or magnesium in the blood can disrupt the cardiac rhythm.
- Medications: Beta-blockers, calcium channel blockers, and other anti-arrhythmic treatments might cause a decrease in heart rate as a side effect.
- Sleep apnea: Interrupted breathing patterns can cause episodes of bradycardia during sleep.
Symptoms of Bradycardia:
Many patients with bradycardia do not exhibit any visible or observable symptoms. When symptoms appear, they may include: especially if the heart rate is only slightly below normal. When symptoms do appear, they may include:
- Fatigue
- Dizziness or lightheadedness
- Fainting
- Shortness of breath
- Chest pain
- Confusion or difficulty concentrating
- Intolerance of exercise
If you have any of the following symptoms and a change in your heart rate, let your doctor know.
Diagnosis of Bradycardia:
Bradycardia is normally diagnosed with a complete medical history, physical examination, and multiple diagnostic procedures, including:
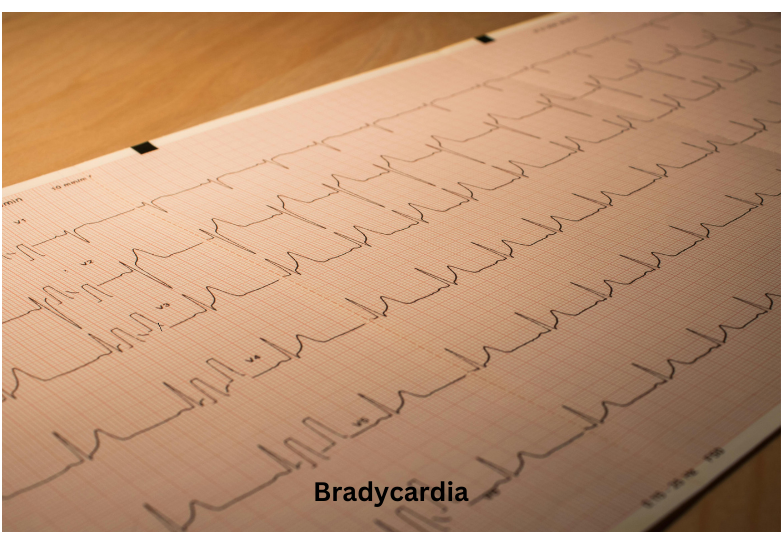
Electrocardiogram (ECG or EKG): This non invasive test examines the electrical activity of the heart and can detect irregularities in heart rhythm, such as bradycardia.
Holter monitor: A portable device worn by the patient for 24 to 48 hours that continually records the heart’s electrical activity, allowing clinicians to detect any intermittent rhythm problems.
Event monitor: These are similar to Holter monitors, but they are worn for a longer period of time, usually up to 30 days, to catch less frequent symptoms.
Blood tests: May include thyroid function and electrolyte levels can be used to detect the underlying reasons of bradycardia.
Sinus Bradycardia
The sinoatrial node (SA) is your heart’s natural pacemaker. It causes electrical impulses to pass through your heart muscle, resulting in a heartbeat.Sinus bradycardia occurs when your SA node sends electrical impulses at a slower rate than normal.
Sinus bradycardia can occur as a natural part of the ageing process. It can also arise due to a number of factors that have been mentioned above, including:
- Adverse effects from specific drugs
- Health issues such as hypothyroidism or sleep apnea.
- Possible causes of heart muscle injury include heart attacks, previous heart surgery, myocarditis, and congenital heart disorders.
How is bradycardia usually treated?
The proper treatment for bradycardia is determined by its underlying cause, severity, and the presence of symptoms. Treatment alternatives may include:
Medications: In some circumstances, atropine, beta-blockers, or pacemaker drugs may be used to help regulate the heart rate.
Pacemaker implantation: A pacemaker is a tiny device that is surgically implanted beneath the skin, generally in the chest, to control the electrical activity of the heart. It continuously monitors the heart rate and sends electrical impulses as needed to maintain a normal rhythm.
Observation: If bradycardia is mild and asymptomatic, a “wait-and-see” strategy may be advocated, with regular monitoring by a healthcare provider.
Lifestyle changes: Living a healthy lifestyle that includes regular exercise, a balanced diet, avoiding excessive alcohol and caffeine intake, and managing stress can assist improve heart health and lower the risk of bradycardia.
FAQ for Bradycardia :
Q. What Is Bradycardia?
A. Bradycardia is a heart related problem defined by an abnormally slow heart rate, usually less than 60 beats per minute in adults.
Q. What is a dangerously low heart rate?
A. Bradycardia occurs when the heart fails to function correctly and develops an abnormally slow heart rate of less than 60 beats per minute. Bradycardia can be fatal if the heart cannot sustain a pace sufficient to pump oxygenated blood throughout the body.
Q. Who is at risk for developing bradycardia?
A. Probably anyone, however the risk increases beyond the age of 65. There are certain persons People under the age of 50 or 60 may develop bradycardia and require a pacemaker.
Q. Can bradycardia be cured?
A. Bradycardia therapy options include lifestyle adjustments, medication changes, or an implanted device known as a pacemaker. If the slow heart rate is caused by an underlying health problem, such as thyroid disease or sleep apnea, treating the medical condition may help to fix the bradycardia.